Diabetic retinopathy is a complication of diabetes mellitus. Diabetes mellitus is a condition in which the body is unable to use and store glucose (sugar) properly. Over time, elevated glucose levels in the bloodstream result in damage to the small blood vessels in the body, particularly in various organs such as the eyes, heart, and kidneys.
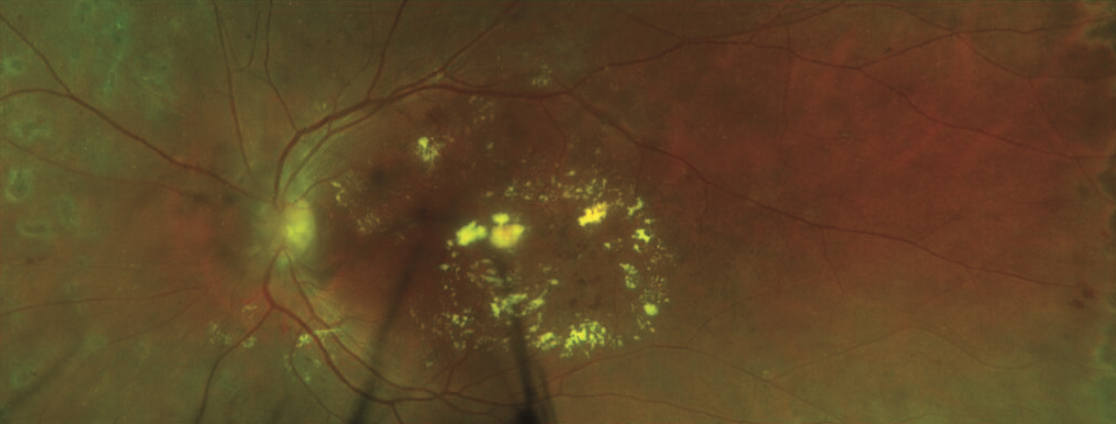
Diabetes can affect the eyes by causing deterioration of retinal blood vessels which may result in diabetic macular edema or neovascularization.
Both conditions can lead to loss of central vision and possibly peripheral vision.
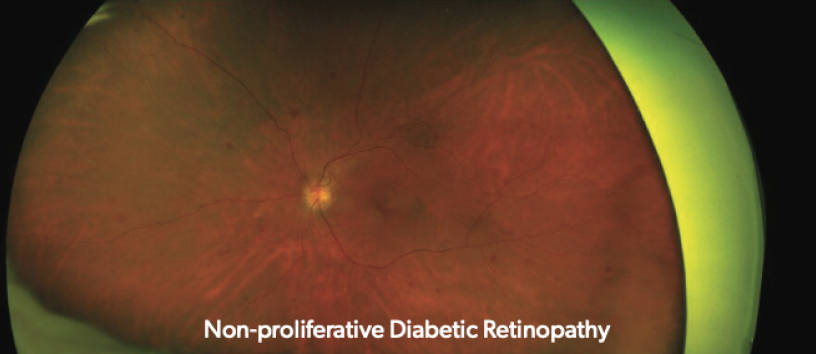
Non-proliferative diabetic retinopathy (NPDR) is the most common form of diabetic retinopathy, accounting for approximately 80 percent of all cases.
NPDR has several stages (mild, moderate, severe) and may be asymptomatic. Diabetic macular edema (DME) can arise at any stage of NPDR and is the leading cause of vision loss among diabetics.
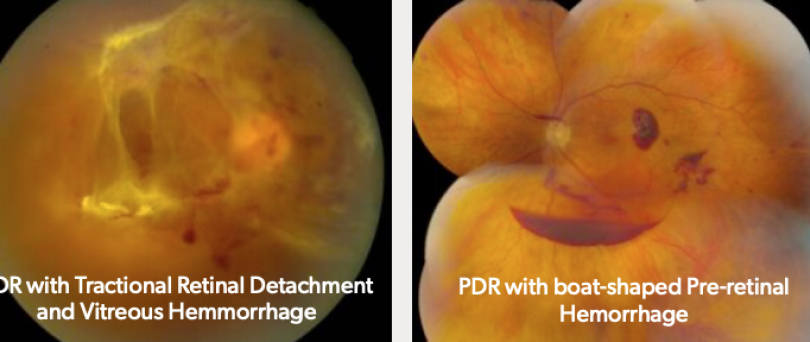
Proliferative diabetic retinopathy (PDR) is characterized by neovascularization. Abnormal blood vessels from neovascularization are fragile and can pull and bleed on the retina, causing vitreous hemorrhage or retinal detachments.
Vitreous hemorrhaging is often sudden and painless and may appear as cobweb-like floaters or block vision completely.
Severe pulling on the retina can result in a retinal detachment, which can lead to vision loss if it involves the macula.
Symptoms of diabetic retinopathy include:
It is important to recognize that symptoms or visual changes resulting from diabetic retinopathy may not be noticeable. Therefore, it is crucial that people with diabetes mellitus have their eyes examined annually by an ophthalmologist.
The longer someone has diabetes mellitus, the more likely they are to develop diabetic retinopathy. After 25 years, nearly all people with diabetes mellitus will show signs of diabetic retinopathy.
The severity of diabetic retinopathy is related to blood glucose (sugar) control. Maintaining blood glucose levels within a normal range can greatly reduce the degree and rate of progression of diabetic retinopathy and other diabetic complications in the body.
Generally, patients should aim to keep the hemoglobin A1C level less than 7. However, the best target level may be higher or lower depending on the patient’s age and other medical problems. The ideal A1C level is best determined by the primary physician or endocrinologist guiding the patient’s diabetes mellitus management.
A complete and comprehensive eye examination is important to assess diabetic retinopathy, including vision testing, eye drops to dilate the pupils, and a complete examination of the front and back of the eye. A driver should accompany the patient during the eye exam as pupillary dilation may create near-vision blurring.
People with diabetic retinopathy may undergo several types of tests to evaluate their condition including:
Intravitreal injections are commonly used to treat diabetic macular edema. They can also stabilize or improve the severity of the underlying diabetic retinopathy. With this treatment, anti-vascular endothelial growth factor (VEGF) inhibitors such as Lucentis, Eylea, Avastin, and Vabysmo are injected directly into the eye.
This procedure is performed in the office and requires only a local anesthetic. Intravitreal injections may need to be administered as frequently as once a month, depending on the severity of diabetic retinopathy and macular edema.
Laser photocoagulation is a standard treatment for diabetic retinopathy and select cases of DME where the macular edema is not located in the center of the eye. A laser delivers a split-second burst of intensely focused light to promote shrinkage of neovascularization or treat leaking retinal blood vessels.
Laser treatments are intended to stabilize and reduce the risk of developing complications from diabetic retinopathy and typically do not result in noticeable vision improvement. Laser photocoagulation is performed in the office setting and is well tolerated after the application of topical anesthetic eye drops.
Vitrectomy surgery is performed in patients with advanced diabetic retinopathy. A vitrectomy is an outpatient surgery usually performed with sedation and local anesthesia. Small instruments are inserted into the eye under microscopic visualization to remove abnormalities such as vitreous hemorrhage and scar tissue. Laser photocoagulation may be performed at the time of surgery; in cases of diabetic retinal detachment, a gas or silicone oil bubble may be placed in the eye to help support the retina while it heals.
As a center of excellence for diabetic retinopathy, the surgeons at Mid Atlantic Retina are intimately involved in the latest clinical trials and new therapeutic approaches for treating this condition.
To learn more about our clinical trials, visit our Research page.
If you have any signs or symptoms of diabetic retinopathy, contact us today to meet with a Mid Atlantic Retina specialist. While there is currently no cure for diabetic retinopathy, our team can work with you to protect your vision and minimize your complications.
Diabetic retinopathy affects the blood vessels in the retina and can, if left untreated, lead...
It’s Diabetic Eye Disease Awareness Month, and a great time to get more familiar with...